Blog
Role of Diet and Lifestyle in Reversing Type 2 Diabetes
For many years, type 2 diabetes has been seen as a chronic disease, one that lasts a lifetime, and one that needs to be “managed” instead of “reversed.” In the last several years, a quiet revolution has occurred in health and nutrition. The story that we are told is not the only story. We now have evidence from scientists, doctors, and the patients themselves that type 2 diabetes is often reversible, not just preventable. The tools to do this are not hidden in some pharmaceutical lab but are simply in your kitchen and your daily habits.
While we are still very interested in understanding how you might reverse the impact of type 2 diabetes at your own pace, it is important to be very clear about what we mean when we reverse type 2 diabetes. Reversing type 2 diabetes means voluntarily bringing blood sugar levels down to a non-diabetic level without medications. This is not a promise for everyone, nor immediate, but for many it is a realistic and achievable goal.
Lets examine how diet and lifestyle play a crucial role in achieving this remarkable health improvement.
Insulin resistance is at the core of type 2 diabetes. The body stops responding to insulin properly, and blood sugar will build up as insulin will not properly take sugar out of the blood. The pancreas will pump out more insulin to combat the blood sugar buildup. Finally, the system burns out.
What could be triggering insulin resistance? While genes may have a small role, it is our choices that will most likely trigger a diabetic state: processed food, too much soda and other sweet drinks, poor sleep, lack of activity, chronic stress, and abdominal obesity do lead to insulin resistance.
Cliché as it may sound, food is medicine. And when it comes to reversing type 2 diabetes, diet is the first line of defense.
Carbohydrates turn into glucose, and glucose raises blood sugar. The body releases insulin to manage blood sugar. When the body receives too many carbohydrates, or when it receives too many poor-quality carbohydrates (like white bread, sugary snacks, soda), the body is overwhelmed at the time that it has to manufacture insulin.
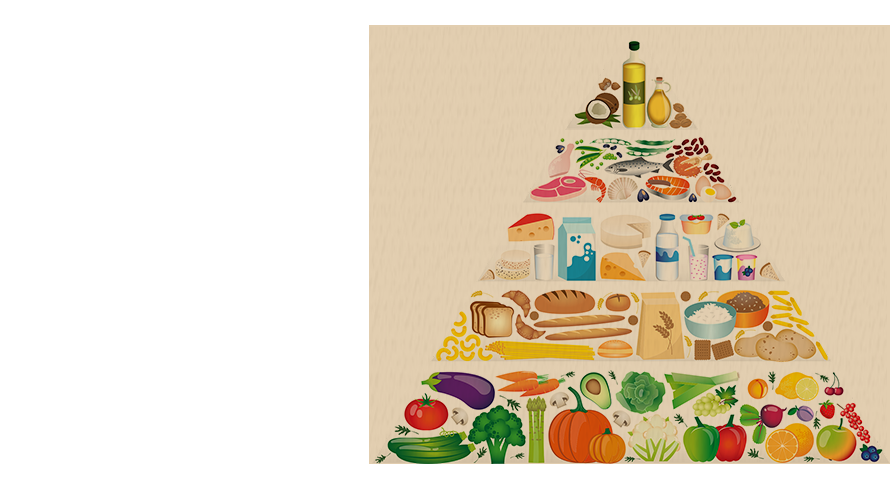
There is credible evidence that a diet that minimizes refined carbohydrates and sugars, and replaces them with complex, fiber-rich sources, whole grains, vegetables, and legumes, offers a sustained improvement in insulin sensitivity. Low-carbohydrate and Mediterranean-style diets, which include a number of healthy fats and lean protein, have also seen dramatic improvements in insulin sensitivity.
For example, just changing a bowl of sugared cereal for breakfast to eggs and sautéed vegetables may allow for a more stable blood glucose level for several hours. Easy entrants, substituting white rice for quinoa or riced cauliflower, can accumulate compelling cumulative effects.
For years, fat was considered bad, but great research has shown us healthy fats (like olive oil, avocado, nuts, seeds) actually enhance our insulin sensitivity and decrease our inflammation. Fat slows down the digestion process. Essentially, it keeps our blood sugar more steady as per meal.
Again, we want to work around trans-fats and highly industrialized oils, and utilize the natural unsaturated fats as allies in blood-sugar management.
Fiber acts like the brake pedal on digestion. It slows the entry of sugar into the bloodstream. Eating plenty of foods that are fibrous like legumes, vegetables, nuts, and seeds (in moderation), and fruit (in moderation) will be very beneficial as well for blood sugar control.
There is emerging evidence that when you eat is just as important, if not more, than what you eat. Intermittent fasting (eating within an 8-10 hour window) may help reset insulin sensitivity and help the body burn fat instead of constantly using glucose for fuel.
This may not seem relevant to insulin sensitivity, but exercise is a bit more than just burning calories to lose weight; exercise helps insulin sensitivity as well. When your muscles contract, they will take glucose out of your blood and decrease your blood sugar naturally.
You dont have to run a marathon for the benefit - studies show that if you briskly walk for just 30 minutes a day will reduce your blood glucose enough to make a difference. Strength training will build muscle, and muscle is very glucose-thirsty tissue. Muscle will keep your metabolism in a good area even at rest when you are not working out.
Did you know? A short walk after a meal can actually reduce post-meal sugar spikes better than many medications, just 10-15 minutes is helpful.
Not getting enough sleep will elevate cortisol (the stress hormone), which will make you more insulin resistant. It will also increase cravings for sugary junk food the next day! Getting 7-9 hours of quality sleep will help you manage your hunger hormones and could benefit your blood sugar.
High stress activates the fight or flight response, flooding your body with hormones that ultimately raise your blood sugar. Mindfulness techniques, yoga, meditation, deep breathing techniques, and even some simple hobbies can be a great way to promote stress management and improve the overall outcomes of your diabetes.
If you have type 2 diabetes, in most cases, losing 5 - 10 % of your body weight could lead to remission! A landmark UK study (the DiRECT trial) suggested that if you sustain a dramatic reduction in calorie intake, and replace food with meal replacements, nearly half of the participants are put into remission for at least 2 years!
Just remember its not about going on diets to lose weight. It is about making small, measured, and sustainable changes to your eating and lifestyle that will leave you with lasting results.
We all know, behavior changes are always easier said than done. Food is comfort, culture, and convenience! Exercise can feel like work! Sleep and stress may feel like a control issue for us!
But heres the encouraging reality: small, consistent changes are far more important than perfection. You are not going to change your entire life overnight. Just make one or two manageable goals:
These small wins add up. You build momentum. And before you know it, your body and health will begin to shift.
It is important to say that while diet and lifestyle can change type 2 diabetes, these should not replace medical guidance. Remember: you will always want to be working with a doctor or dietitian, especially if you are on medications. As your health improves, you may be able to decrease medications (we hope that is a good problem to have!).
For too long now, type 2 diabetes has been seen as a one-way street. Now we know differently. Your daily habits (what food you put on your plate, how you move, how you take time to release stress and how you protect your sleep) can change the wheel.
Reversing type 2 diabetes isnt some medical miracle for the lucky few — it is a possibility for millions that choose to take control.
The journey is not easy. But it is possible. And it starts with one choice today.
Disclaimer: This article is for informational purposes only and does not substitute medical advice. Always consult your healthcare provider before making major lifestyle changes.